Watch my discussion with Brian McAlpine of Bernoulli Health on Continuous Surveillance Monitoring
Recorded Tuesday, June 26, 2018 – 1:00 PM – 2:00 PM EST (10:00 AM – 11:00 AM PT)
The Definitive Guide to Surveillance Monitoring
Using surveillance monitoring to monitor patients at risk of a deteriorating clinical condition is a growing need in almost every hospital. Here's why, from a previous blog post Monitoring Currently Unmonitored Patients:
Every hospital has some unmonitored patients that could benefit from being monitored. Patients on pain medications, especially PCA pumps, should be monitored. According to the literature, almost half of all cardiopulmonary arrests in hospitals are unwitnessed. While the survival rate of witnessed codes is 22%, the survival rate for unwitnessed codes is just 1%. Increased monitoring can reduce adverse events, improve outcomes, reduce length of stay, and minimize legal liability.
Patients with clinical deterioration have resulted in failure to rescue and unwitnessed codes for years. Each occurrence is a very distressing event, for staff as well as family. Let's review past approaches to this challenge to better understand the new surveillance monitoring product category:
- In the past, when the attending physician felt a patient was at risk of deterioration the patient was placed in the telemetry unit. This was because telemetry was the lowest acuity unit with monitoring, even though the patient did not meet unit admission criteria. This resulted the telemetry unit becoming a common hospital patient flow bottleneck for the hospital. Consequently, telemetry beds filled up, sometimes resulting in the hospital going on ambulance diversion.
- The utilization of surveillance monitoring continued to grow. To mitigate the telemetry unit patient flow bottleneck problem, some hospitals adopted what are called variable acuity units or universal patient rooms. Now when a patient's condition deteriorated, rather than transferring them to a higher acuity unit, the level of care is increased to support an appropriate clinical intervention to arrest the deterioration. This higher level of care typically included patient monitoring and perhaps a lower nurse to patient ratio. The goal is to keep patients on their service unit whenever possible and avoid the extended length of stay that results from transferring patients between units.
- Alternatively, many hospitals adopted basic house-wide surveillance monitoring without the formal conceptual framework of variable acuity units. The ability to monitor patients in most or all patient care areas was implemented so that patients could be monitored anywhere. Obviously, higher acuity patients would be in higher acuity units that already have monitoring. Most patients in the house-wide monitoring scenario are patients at risk of a deteriorating clinical condition.
In all three of these examples the monitor used was almost always the telemetry pack.
Telemetry Monitor Limitations
For the past 15-20 years, the patient monitor that has come closest to meeting surveillance monitoring requirements is the telemetry pack. Despite being the "best" monitoring solution for patients at risk of a deteriorating clinical condition, telemetry packs were far from perfect.
At about $8,000 per monitor, telemetry packs are considerably less expensive than the typical multi parameter patient monitor. They are well tolerated because of their size and because they're patient worn. All the cables can be placed out of the way underneath the patient's gown. The result has been the frequent purchase of telemetry packs — not for patients with arrhythmias, but for patients at risk of a deteriorating clinical condition.
The fact is, telemetry packs really fall down on the job of surveillance monitoring. The ideal physiological parameters for determining clinical condition deterioration are the common vital signs, especially respiration rate, blood pressure, heart rate, and SpO2.
Arrhythmias captured via telemetry ECG waveforms are not early indicators of clinical deterioration. Patients typically pass through deterioration into decompensation and crisis before they start to throw arrhythmias. At this late stage it is too late for an early and inexpensive intervention - the kind with the best outcomes and highest survival rates.
The principal physiological parameter provided by telemetry, ECG, is also a major source of alarm fatigue. The multiple ECG sensor require skin prep, careful application, maintenance and replacement to minimize leads-off and false positive alarms. These ECG sensors are also very susceptible to motion artifact, generating alarms when patients roll over in bed, brush their teeth, etc. ECG and arrhythmia parameters are also a common source of transient nuisance alarms.
Many older telemetry packs still in use do not have any kind of display or indicator of an alarm condition on the monitor itself. This means caregivers must depend on a central station to keep tabs on patients. And because caregivers have little time to hang out at the central station, central monitoring with monitoring techs or alarm notification systems may be required to make sure alarms receive timely response. Increasing alarm volumes, using multiple message panels and slave displays are common — but not very effective — methods to mitigate alarm notification limitations.
In many cases, using telemetry packs has resulted in alarm fatigue. Contributors include numerous ECG sensors, motion artifact, and ineffective mitigations for limited alarm notification capabilities. All this results in a high volume of alarms, many of which are non-actionable nuisance alarms.
New Surveillance Monitoring Solutions
With the history surveillance monitoring above, let's now turn our attention to the new surveillance monitoring solutions currently being brought to market.
The first alternative to telemetry packs were SpO2 monitors. The Medtronic/Covidien/Nellcor VitalSync solution and Masimo's Patient Safetynet solution have been adopted by many hospitals for surveillance monitoring. However, these solutions also have limitations: patient monitors too large to be patient worn, limited mobility and a propensity for false/positive or nuisance alarms. There is also some question whether SpO2 is the single optimal parameter for identifying patients with a deteriorating clinical condition.
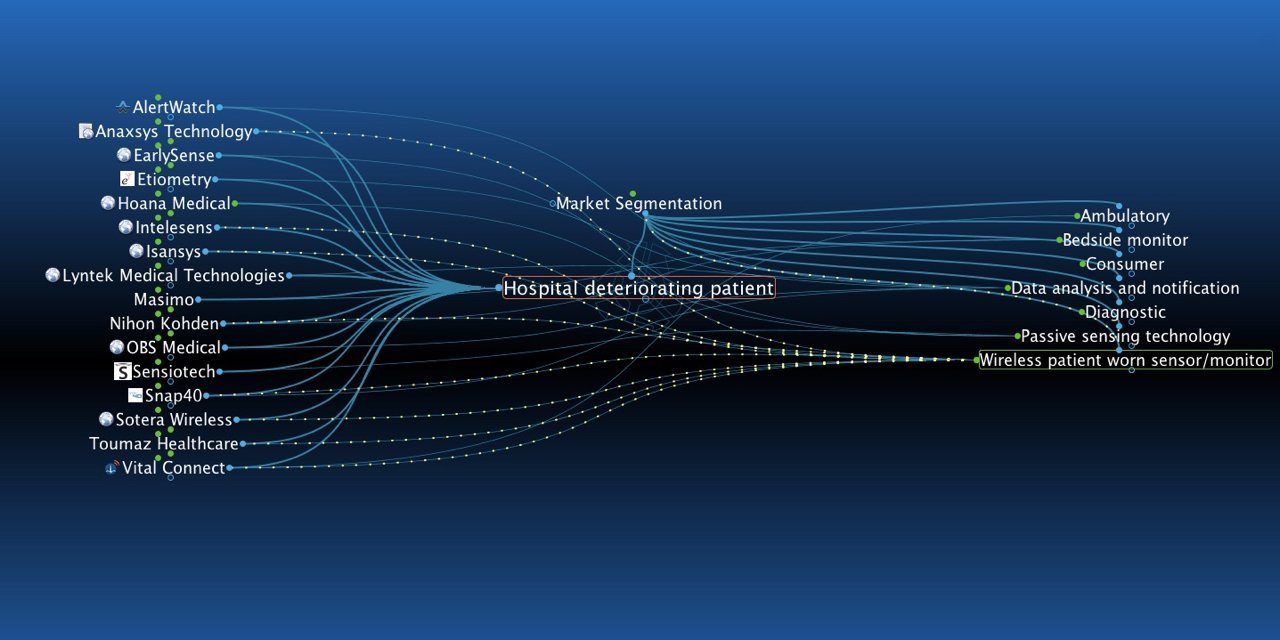
Over the past 10 or so years, a growing number of entrepreneurs have recognized the opportunity resulting from this gap between clinical need and available solutions. I'm currently tracking about 25 surveillance monitoring companies that make claims to identify hospital patients at risk of a deteriorating clinical condition. When I posted the first version of this blog post 2 years ago, there were 17 vendors on my list.
There are some very compelling surveillance monitoring solutions available today. At this relatively early stage of the market's development, there is wide variation among vendors in their basic approach to surveillance monitoring and the breadth and depth of overall solutions. Let's consider the basic surveillance monitoring process as a framework to consider thee new solutions.
The Basic Surveillance Monitoring Process
The goal of surveillance monitoring is to avoid failure to rescue and unwitnessed codes by detecting patients with a deteriorating clinical condition. Whether using patient monitors and nursing vigilance or automating the process with data analysis and automatic alerts, the basic process is the same:
- Patient physiological data is collected via instrumentation and perhaps direct observation
- That data is analyzed to determine whether the patient is deteriorating
- A decision is made that deterioration is occurring
- The care team is notified of this deterioration and a clinical intervention is planned and executed
To varying degrees, surveillance monitoring solutions facilitate or automate the above process. Let's look at how this process is translated into a solution architecture, used by many of today's surveillance monitoring solution providers.
Surveillance Monitoring Solution Architecture
Surveillance monitoring solutions are, for the most part, built out of the same series of functional blocks that make up a solution architecture. We will describe each functional block and then consider vendors focused on specific blocks.
Everything starts with the patient, data from medical devices and patient data in the EMR. Physiological data is collected by sensors connected to a patient monitoring device. Further contextual data can be collected by therapy delivery devices.
The EMR provides patient demographics: ADT, patient history, diagnosis, recorded periodic vital signs data (patient chart and flowsheet), potentially relevant data on medications (electronic MAR), and diagnostic test reports (Results Reporting).
Acquired data goes into some sort of data management system that can range from a scalable high-fidelity near real-time medical device data system (MDDS) to a smaller and simpler database with abstracted historic data.
A clinical decision support system (CDSS) then applies the data to algorithms to make recommendations, generate alerts/alarms, and possibly render or recommend a diagnosis. The final functional block is some sort of analytics or reporting module.
Besides the EMR, another ancillary system often provided by third parties is a messaging system that communicates alerts and alarms generated by the surveillance monitoring system to caregivers and clinicians.
Many of these types of systems also provide some sort of central station client apps for remote surveillance, retrospective event review, data visualization and other features.
Attributes of a Surveillance Monitoring Solution
Many of the current surveillance monitoring solutions include patient monitors intended to detect patient deterioration. Here's my list of product attributes:
- Cost effective — Increasing the number of monitored patients is expensive. Cost effective monitors are essential for surveillance monitoring.
- Well tolerated by patients — These patients are low acuity, fully conscious and often ambulatory. They don't want a bunch of tubes and wires between them and a wall or pole mounted device. Nor do they want something that's constantly alarming and keeping them awake.
- Efficient for caregivers — Surveillance monitoring for deteriorating clinical conditions must be easy to apply to patients, require minimal maintenance of sensors and the device, generate actionable alarms only, and address the back-end function of alarm notification and response.
Many surveillance monitoring solutions are built around new monitoring technology intended to meet the high level attributes above. Some surveillance monitoring solutions use existing patient monitors already in use in the hospital.
Surveillance monitoring captures physiologic data through various types of monitors: multi parameter bedside monitors, spot vital signs monitors, wireless patient worn monitors or remote sensing monitors. The first two categories of monitors are found in any hospital; the final two categories — discussed below — have been brought to market intending to address the needs for surveillance monitoring.
Wireless Patient Worn Monitors
Wireless patient worn solutions can be divided between reusable miniaturized monitors strapped to the patient — typically an arm or wrist — or band-aid style disposable units. Nihon Kohden, Sotera Wireless and Masimo (Radius-7) are good examples of the reusable miniaturized monitor. The Sensium and Vital Connect devices are examples of the band-aid disposable approach. The disposable Intelesens device is a bit of a hybrid, being mostly a disposable with a small reusable component. The band-aid approach has the advantage of including the ECG sensors as part of the device. Miniaturized monitors, and some band-aid solutions, use separate sensors that are also attached to the patient.
Companies in this category include (in alphabetical order):
- Anaxsys
- Intelesens
- Isansys
- Masimo
- Nihon Kohden
- Respiratory Motion (beside monitor)
- Snap40
- Sotera Wireless
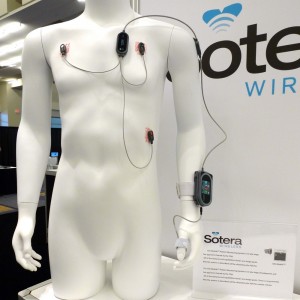
Sotera Wireless Visi Mobile patient worn monitor
- Sensium
- Vital Connect
Parameters typically include heart rate, respiration, ECG (but not arrhythmias) and may include SpO2, NIBP, temperature and motion. Some solutions offer more novel parameters such as beat to beat heart rate variability. Motion can be used to provide a number of features: to filter motion artifact to reduce nuisance alarms, bed exit alarms, fall detection, patient position for evaluating certain physiological parameters and bed turns to avoid bedsores.
Passive Remote Sensing Monitors
Passive remote sensing monitors are completely noninvasive and typically collect patient data from several inches to several feet removed from the patient. Most passive sensing technologies used for this application use electromagnetic energy beamed at the patient, from which a reflected signal contains physiological data that is extracted and used to monitor the patient.
Companies in this category include (in alphabetical order):
The physiological parameters acquired by this technology tends to be limited to heart rate, respiration and perhaps motion. The sensors that collect patient data for these solutions are made up of a pad or plate that is placed under the patient, on top of or under the mattress. These systems sometimes include optional patient worn sensors for parameters like SpO2.
The motion parameter can be as simple as noting unspecified patient movement, or can be used to report patient agitation scores, bed turns (to avoid bed sores), and perhaps more accurate bed exit alarms.
Therapeutic or Life Support Devices
Infusion pumps, ventilators, intra-aortic balloon pumps, dialysis and other therapeutic devices can transmit data about configuration, therapy delivery, alerts/alarms and other data. This data can be useful in providing additional contextual information for identifying deterioration or diagnosing other conditions such as sepsis.
Currently most surveillance monitoring systems do not acquire data from these devices.
Data Management System
Once all this data is collected, it needs to be stored and managed. Again, this can range from a high fidelity near real-time database that is highly scalable, to a simple relational database. The former represents some serious technology development and can be a standalone product or strategic feature in a broader solution. The latter, simple relational databases, are off-the-shelf commercial or open source software that are an essential part of almost any kind of information system.
Companies in this category include (in alphabetical order):
- Bernoulli Health
- Excel Medical
- True Process (their ViNES product)
Clinical Decision Support System
If it was easy to identify the deteriorating patient and make the call to intervene, this growing market segment would not exist. The approach to the deteriorating clinical condition challenge is to apply specialized algorithms to a patient's physiological data to identify clinical deterioration in a reliable and unambiguous way.
More enterprise focused clinical decision support solutions include indications for use beyond clinical deterioration to include things like tight glycemic control, sepsis and other indicators and diagnoses. Clinical surveillance monitoring systems focused on identifying patients with a deteriorating clinical condition may or may not include a clinical decision support system and would be considered more of a point solution.
Companies in this category include (in alphabetical order):

This OBS Medical display shows the results of data analysis on patient data.
- AlertWatch
- Bernoulli Health
- Decisio Health
- Etiometry
- Jvion
- Lyntek Medical Technologies
- OBS Medical
- PeraHealth
Each of these solutions produces an early warning score or index that is used to indicate a deterioration of the patient's clinical condition. Once a predefined threshold is reached, the system flags the patient as having a deteriorating clinical condition.
Across the different solutions, each score is different as is the algorithm that generates the score. These algorithms take the common parameters found on bedside patient monitors, purchased separately, such as, heart rate, ECG, respiration, SpO2, and temperature. Some algorithms also take into account caregiver's patient assessments and other clinical data found in the EMR.
Client Applications
Surveillance monitoring systems use various client applications to allow users to interact with the system. This starts with patient context, where patients are registered in the system and the surveillance process is initiated. As data is collected and the patient's condition is evaluated, visual feedback of the patient's status is displayed. Changes in the patient's condition is also indicated via a client application.
Client applications can also include retrospective review of patient data (based on alert or monitoring events or time periods). Some systems include novel ways to visualize the patient's condition and track it over time.
Client applications are intended to be run on desktop or laptop PCs and/or mobile devices.
Ancillary Systems
Certain ancillary systems are often required to provide a functional and complete surveillance monitoring solution. The two most common ancillary systems for this application are the EMR and an alert/alarm messaging system.
The most critical ancillary system is the electronic medical record. As noted above, the EMR provides information for patient context, non-medical device data used to identify clinical deterioration (caregiver assessments, diagnostic test results, medications, etc.), and with some solutions, vital signs captured by vital signs monitors and entered into the EMR.
Every surveillance monitoring system must have patient context to properly identify the right data with the right patient and manage the patients on the surveillance monitoring system (see this blog post on the Patient Context Workflow for more).
A few surveillance monitoring solutions include a messaging feature to communicate alerts and alarms directly to responsible caregivers and clinicians. Most other systems use a central station and/or an interface to a third- party messaging system to convey alerts and alarms for clinical deterioration.
Solution Architecture Summary
Surveillance monitoring is a growth market due to a clear market need to reduce unwitnessed codes and avoidable failure to rescue sentinel events. Some of these solutions can also be used to implement remote ICUs, facilitate clinical research, capture data for training artificial intelligence algorithms and other activities that require a rich set of medical device data.
Any growth market has to work through the process of determining the optimal solution for their market need. There are a variety of different ways to solve the surveillance monitoring challenge of identifying patients with a deteriorating clinical condition. Which of these approaches will prove to be widely adopted by the market is yet to be determined.
As the market matures, options and approaches to surveillance monitoring will likely narrow. Until that time comes, buyers will have to consider which of the answers to the above questions best fit their needs and situation. The "best" answers to the above questions will also be influenced by the preferred solutions under consideration.
This wraps up the review of a typical solution architecture for surveillance monitoring. Now we will delve into issues around the state of the market and challenges in vendor selection and system implementation and adoption.
Whole Product Solution
All the products, features and services needed for a complete working solution, capable of fully meeting user requirements, are known as the whole product solution.
A consequence of the relative immaturity of the surveillance monitoring market is that vendors tend to have various gaps in their whole product solution. As a result, a complete surveillance monitoring solution often includes functional building blocks from more than one vendor. That gaps exist in single vendor solutions is less an issue than identifying which gaps, and ensuring those gaps are filled with something appropriate.
The functional building blocks of the solution architecture described above are a good starting point for defining a vendor's whole product solution. Make sure to determine which of the building blocks are covered by a vendor's solution. Also bear in mind that there are often substantial functional differences between different vendor's implementation of a particular block in the solution architecture. These functional differences may or may not be important when evaluating a vendor's overall solution, depending on your unique needs and situation.
Besides evaluating the solution architecture, the issues raised in the Purchase Challenges and Implementation Challenges below describe additional items required for a whole product solution. These two challenge areas revolve around services starting with the vendor providing basic training, an implementation project plan, advice on clinical indications (for who should be monitored), a sample order set for the CPOE system, and sample policies and procedures for using the new solution. Systems integration between monitoring and therapeutic devices, the EMR, and any portions of the solution architecture provided by third parties must also be included.
Purchase Challenges
With 20+ different surveillance monitoring solutions available, determining the solution with the best fit for your situation definitely qualifies as a challenge — especially when so many of the solutions take such unique and different approaches to the problem of surveillance monitoring. Clinical surveillance covers everything from remote ICUs, to wide ranging clinical decision support, to the actual detection of clinical deterioration. The key here is to properly assess your short and long term clinical and patient safety needs to narrow the scope of potential solutions.
Besides clinical and patient safety objectives for your surveillance monitoring system, it is important to take into consideration how a specific vendor's solution impacts governance. Every provider organization has their strongly held preferences and organizational dynamics regarding essential physiological parameters, what constitutes deterioration and how caregivers and clinicians work together. Each surveillance monitoring solution is designed based on certain assumptions regarding governance, group preferences and dynamics. An otherwise perfectly good solution may not work in an environment based on different or incompatible governance, group preferences and dynamics.
Finally, be sure to consider the necessary systems integration and infrastructure for your chosen solution. If your preferred whole product solution requires more than one vendor, setting systems integration expectations with all parties prior to purchase is a must. IT infrastructure can become a critical issue when your surveillance monitoring vendor of choice provides a wireless patient monitor. Care must be taken to ensure your existing wireless infrastructure is designed to support this new application, and if not, a pre-purchase assessment must be undertaken to determine the scope of any network remediation required for optimal performance.
Implementation Challenges
Perhaps the biggest challenge to adopting surveillance monitoring solutions is implementation. Like a lot of new point-of-care technologies, much depends on successfully changing user behaviors and gaining near-universal adoption. Such a high bar is difficult, and requires a solid plan and considerable effort to drive the needed change and adoption.
One of my favorite sayings is that everyone wants to automate, but nobody wants to change the way they do things. The reality is that the very act of automation necessitates changing the way things are done. This issue is embodied in the kinds of governance changes that are required to implement surveillance monitoring solutions.
At a high level, governance impacts:
- Who orders surveillance monitoring and why
- What patients get monitored
- Who (or what) calls clinical deterioration
- What interventions are appropriate and in what circumstances
- The role of Rapid Response Teams when surveillance monitoring is adopted
- Ongoing use of performance data for Continuous Quality Improvement and other management efforts
In most hospitals, surveillance monitoring is a house-wide deployment. In those cases, governance should be consistent house-wide. Any units with variations should be limited and clearly justified due to data regarding their patient populations and clinical factors.
Every provider organization is unique in how preexisting governance is defined, and the appetite among individuals and groups for certain types of change. This is an iterative process, requiring facilitation and guidance. Matching an organization's unique situation with a solution that can support the preferred governance approach is a must.
As noted above, the flexibility to support certain approaches to governance or specific policies and procedures can vary among surveillance monitoring solutions. Consequently, governance issues should be addressed early on in the needs assessment and vendor selection processes. This way the status quo can start to be questioned, consensus can begin to emerge, and a vendor of choice can be selected that is consistent with your specific governance and group dynamics.
Wrap Up
This has been our comprehensive look at surveillance monitoring for patients at risk of a deteriorating clinical condition and related indications. We've looked at the need for and evolution of surveillance monitoring over time and why new specialized solutions have been brought to market. We next considered the solution architecture and the types of surveillance monitoring solutions that have evolved and some of the specific companies who have developed solutions. We ended with a brief survey of the whole product solution, along with the capabilities and services needed to successfully implement and use surveillance monitoring.


Who have you see exhibiting traits that address the “whole product solution?” If you haven’t been looking at Philips Healthcare, I would take a closer look. They have wireless monitoring, patient monitors, data analytics for predicting deterioration, and the ability to integrate into the EMR. As hospitals dip their toes into this new ocean of solutions, I think it would be important to partner with a single solution to maximize the dwindling profits in the General Care areas of a hospital. It definitely needs to scale as I am sure most hospitals would have a hard time purchasing the total solution or if one of the partial solutions mentioned above can’t meet the basic criteria of sending vitals into the record. Thoughts?
PezMan, I’ll be getting more into the whole product solution and various manufacturer trade-offs in subsequent posts. However, because Philips, like their direct competitors (other than Nihon Kohden), do not have a device intended to monitor patients at risk of a deteriorating clinical condition, I’m not planning to include them.
While one can certainly use a conventional pole or wall mounted multi parameter patient monitor in this application, the costs tend to be higher and patient acceptance lower compared to the patient worn or the passive sensing devices.
Good article. I would think it would be critically important to understand which CDS solutions use EMR data, and which are using more sophisticated analytical approaches, such as ML/Deep Learning. Have you done any analysis of this or do you plan too?
Michael, think of a CDSS matrix where data sources is one axis and analysis is the other. Some CDSS use EMR and other HIT app data, some use medical device data (either periodic or near real-time) and some use both data sources. On the “decision support” axis, the kinds of decisions sought and the efficacy in reaching accurate timely decisions is key. Whether a system uses a deterministic rules engine or a probabilisitic AI approach strikes me as less important.
Things are still very early on with AI, though I do imagine that AI will eclipse rules engines at some point. One of the biggest things holding back all AI approaches is the lack of data to train the algorithms. Sure there’s plenty of abstracted retroactive EMR and medical record data, but finding big rich databases filled with physiological data remains a challenge.