Wireless changes everything …
I have been watching the evolution of wireless bedside medical device connectivity for several years now. It is now fairly common for medical devices to communicate wirelessly and most hospitals now have the requisite Wi-Fi networks installed and operational. In fact, the saturation point of WLAN adoption in US hospitals has been reached as the numbers are quickly approaching 90% of all US hospitals.
But this posting is not about Wi-Fi or other wireless technologies used in medical devices. Rather it is about additional connectivity considerations beyond the actual wireless connection of the device to a network. Regardless of the wireless connection technology or standard used, wireless changes everything when it comes to connectivity.
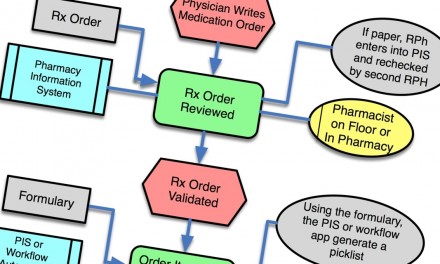
And as Tim Gee notes, clinician workflow is a key component of the definition of connectivity. But from an end users perspective - meaning the clinician at the bedside - point of care workflow is often the determining factor in the acceptance and adoption of connectivity solutions.
Two of the Most Common Myths About Wireless Connectivity
Myth #1: The first myth - actually a very common misunderstanding related to Wi-Fi enabled medical devices is -- "if the device is 'on the network' then the connectivity problem is solved.”
Myth #2: The second myth related to the wireless enablement of serial medical devices is the thought process that says -- "Just eliminate the serial cable by putting a wireless adapter on the serial port -- problem solved."
Nothing could be further from the truth. In fact, more connectivity problems are actually created than are currently solved by wireless medical devices. This may seem like a fairly bold statement - so let’s explore this further and see if these myths can be dispelled.
First of all, for clarification, it is not wireless per-se that causes connectivity problems. Rather it is the fact that wireless enables mobility and therefore the overall connectivity problem becomes more complicated. Once a medical device is enabled for mobile connectivity, the management of patient context becomes a key requirement and an enabler for seamless integration. Here, patient context refers to the linking of a medical device's data and alarms to a verified unique patient ID. And this is where clinical workflow comes into play.
For device data integration, the traditional method of linking device data to a location-based identifier - such as a bed label or room number, works fine for stationary devices. For example, a patient monitor bolted to the wall of an ICU room. However, because the patient can move (i.e. ambulating) or be moved (i.e. transport to radiology) and the medical device can also move without losing connectivity (enabled because of wireless), then the location-based identifier quickly becomes very problematic. In fact, it creates a potential unsafe condition. The risks to the hospital are misidentification of the data and the resulting potential of having the data end up in the wrong patient's record or the device's alarms going to the wrong caregiver. In fact, in the U.S., the Joint Commission is thinking along the exact same lines. The 2009 National Patient Safety Goals spell this out in their very first stated goal.
Use at least two [patient] identifiers when providing care, treatment, and services. And performance element # 5 under the first goal states: The patient’s room number or physical location is not used as an identifier.
In dispelling Myth #1 - consider a wireless ventilator or IV pump connected to the enterprise WLAN. Without patient context, the device is in essence "running blind" from a connectivity and integration perspective. Without knowing who the actual patient is - how do you know where to send the data or alarms? The answer is you can't, at least reliably you can't. Sure the device can communicate to its own dedicated gateway server via the wireless network, but integration with external systems is limited without patient context.
And Myth #2 is really just a variation of Myth #1. Once you eliminate the serial cable, you essentially have not solved the connectivity problem until you consider how patient context will be established and managed.
Managing Patient Context
From a patient safety perspective, the safest way to solve this problem is to establish patient context at the patient's bedside. This is where managing patient context for medical devices intersects with the more common industry term - Positive Patient ID or PPID. Here is where things get really interesting because establishing patient context is all about the clinical workflow and less about the technology. But some technology choices enable better workflow than others -- as Tim describes in this post. In future posts, I will explore some of the real world issues and challenges with patient context and workflow at the bedside. To give you a preview - here are a few things to consider.
- Is the use of barcoding technology really the best method for establishing and managing patient context? Or are there alternatives that enable improved workflow and positively impact patient safety?
- If a clinician starts establishing patient context for wireless/mobile medical devices, should they do it the same way for non-wireless devices as well?
- Can't an interface to the ADT system solve the issue by providing the patient ID for the patient that is in the bed?
- How much can you ask a nurse to do at the bedside before they find workarounds or refuse to do any more?
- Doesn't the medication administration process involve a form of establishing patient context - i.e. the 5 rights process?
- What other clinical processes involve the management of patient context or verification of PPID?
- Is patient context the only concern? Wouldn't clinician context be important? How about location context?
Just about anything is technically possible, but the real question is - will the nursing staff actually use it? Let me know your perspectives – agree or disagree. Do you see wireless causing these types of problems today?


This is a very good start Brian as it is a complex problem revealed by my first hand clinical experience this week. When my wife was admitted for surgery she was given a RTLS (Sonitor), tag so she could be tracked during the surgical procedure to PAR (post anesthesia recovery). This somewhat automated at least patient context during this procedure and to the PAR. However, since it did not continue past the doors of the PAR, then my wife left the PAR the value of their RTLS dropped off the cliff.
For example, no one could tell me when she left PAR, or when she arrived in her room. All this points out that in the RTLS world, this has to be enterprise wide. Then to the med-surgical area, (this hospital is very advanced as in the top 100 Most Wired and Wireless Hospitals). Everytime a medication was delivered they did use a “wireless” scanner, (actually imager). I asked the clinicians, (some of who worked there for 20 plus years), what they thought. Initially some resistence, but they felt this has actually helped them relieve some anxiety of the care process. However, I did not seen anyone “image” the infusion pump to associate or dissassociate.
Great presentation, Brian. It is a very complex and frightening problem for all persons involved, from the patient to the caregivers. One of the points you mentioned that goes beyond the risks to patient safety and accuracy in caregiving is the inherent problems of increasing “work” at the bedside for the clinicians. Acceptance of technology is one hurdle, usefulness of technology that actually enhances the care process, rather than adding steps to administration of care, is another. It’s clear the industry needs to provide a safe & relatively seamless method to provide patient context, presence, and accurate content of information. No small order, there….