My February, 2010 discussion of Meaningful Use (MU) (found here) addressed the then proposed 25 elements by which an EMR/EHR (hereafter EMR) would be judged in order to determine if it met the funding standard for MU under the U.S. federal incentive program regulations. Note that in this regard an EMR must be capable of MU, and then MU must be actually achieved by the end user. Capability is established by vendor certification.
As is perhaps common in the sequence of proposed and revised federal regulations, that the scope of the 25 elements received a degree of adverse response that centered on the assertion that they were overly demanding, i.e. we want the money, we just don't want to work that hard to get it. As a result the 25 required elements were reduced to two sets of requirements in what is now called Stage 1. The first set is 15 required elements while the second is a "menu" of 10 additional elements of which 5 must be chosen.
An overview of the Stage 1 15 requirements and the menu of 10 can be found here. In short, the required elements are (1) computerized medication order entry, (2) drug interaction checks, (3) maintenance of a patient diagnosis list, (4)electronic prescription transfer, (5) maintenance of a current medication list, (6) maintenance of an active allergy list, (7) recording demographics, (8) recording vital signs, (9)recording smoking status, (10) reporting of clinical quality measures to CMS, (11) implementation of one clinical decision support rule (see below), (12) providing patients with electronic copies of their records and (13) with a clinical summary for each office visit, (14) enable information exchange, and (15) protect electronic health information.
The menu items are(1) implementing drug formulary checks, (2) incorporation of clinical lab results, (3) multi-patient data access for quality improvement and research, (4) patient reminders, (5) timely patient electronic access, (6) targeted patient education, (7) medication reconciliation on transferred patients, (8) summary records for outbound transfers, (9) transferable immunization records, and (10) transferrable public health data.
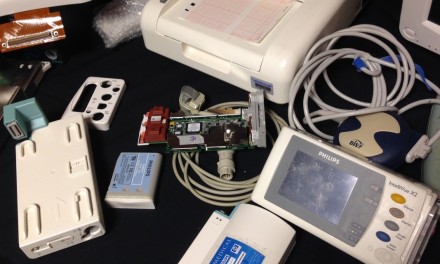
As Tim Gee has pointed out elsewhere, from the connectologists' perspective these requirements are relatively bland in that they in general do not require that any inputs be delivered from medical devices or other systems directly into the EMR. For example, it might be helpful in meeting requirement 8 to have a vital sign system that automatically inputs the data as obtained. However it is equally acceptable for current MU purposes that someone write down the vital sign information and then enter it manually. It is also clear that there is no current requirement for therapeutic medical devices to provide a periodic or continuous data stream to the EHR. These leave for another day all of the challenging questions associated with such transfers including why you want to do it in the first place, how much data is that to move and store, and how do you associate and de-associate patients and devices.It has also been noted that the standards are silent with respect to the inclusion of imaging. Of course these standards and requirements reflect the minimum that must be included in MU. There is no maximum.
Returning to decision support (DS) (element 11), I have discussed DS in these pages previously (here). DS is defined as an HIT function that provides general and person-specific information, intelligently filtered and organized, at appropriate times, to enhance health and health care. Interestingly here drug-drug and drug-allergy interaction alerts are explicitly not satisfactory for meeting this rule, possibly because those are too easy and more-or-less readily available.Without the inclusion of drugs, which some vendors had seen as an easy route to DS, it isn't clear where the DS system will come from, or how it will be shown to satisfy reasonable assurances of proper domain definition and exclusion, whether or not clinicians are actually supposed to rely on the DS "suggestions", and is a DS an FDA regulated medical device.
The above was background in a sense, because there is now a Working Group proposal for MU Stage 2 which was made available in January, 2011 with a request for comments. For the most part this proposal refines issues with Stage 1 elements and increases the performance standard required for objective proof of compliance. A few new components have also been added that address eligible hospitals (EHs) as opposed to eligible professionals (EPs). Note that here eligible means eligible for federal funding. For example, new in the Stage 2 proposal for EH's is visits having electronic EP notes, automatic tracking of medication orders, listing of all care team members, and a patient accessible web portal. For EPs there is online secure patient messaging and notation of the patient's preferred means of communication. A reasonable expectation is that the Stage 2 proposals will be commented on, massaged, and somewhat reduced. Both vendors and end users have to be challenged by evolving requirements that will require both product updates and new work processes, including having clinicians actually look at information contained in the EHR. Still ignored for the most part is whether EHRs are medical devices subject to FDA regulation, as discussed by Tim here.The timeline for implementation of Stage 2 is 2013. There is also a not yet developed Stage 3 set for 2015.
There is a perhaps not a surprising parallel between the role out of the MU requirements (25 down to 15 +5 of 10) with more to come, and the FDA's ongoing review of its 510(k) process. In the latter the initial FDA report had 55 recommendations which, after much collective industry gnashing of teeth (with some congressional co-gnashing), was reduced to 25, with others referred to the Library of Medicine which is also studying issues with 510(k)s. There must be a guideline someplace that suggests proposing too much so that you can reduce the proposal after adverse public comment, giving the appearance of both listening and relief. Of course reduced requirements raises other's ire, who think that the end result has been too watered down.



Would you need to meet Meaningful Use; for a Home Telehealth System?
Hi Bill,
Just wanted to bring to your attention that we just published an article on meaningful use. I’d love to get your take on the article.
http://www.mddionline.com/article/meaningful-use-door-innovation
RESPONSE: The answer to both comments depends in part on the difference between capital M, capital U Meaningful Use, and plain language small m, small u meaningful use. There are many medical device/IT combinations that can be (potentially) meaningfully used, but they do not constitute MU as presently defined because they are not within the scope of the requirements for the federal incentives for the the adoption of an EHR/EMR by an eligible profession (EP) or eligible hospital (EH). Working to get the definitions of MU changed is fine, and part of the process. But that is different from thinking that a single function device, or home telehealth system, falls under the current or presently proposed requirements, or the associated financial incentives.
“The Age of Meaningful Use”, a message from Dr. Blumenthal, the National Coordinator for Health Information Technology, was posted today. Taking a somewhat broad view of meaningful use, Dr. Blumenthal notes that: “meaningful use†is a shorthand for three things: 1. An incentive program, rewarding not only deployment of EHRs but also their effective use for patient benefit; 2. A new national infrastructure to support deployment and beneficial use of EHRs; and 3. A vision for the evolving, dynamic and optimal uses of information to support health and health care improvement – the tip of the spear for an information-powered leap in the quality, safety and effectiveness (including cost effectiveness) of our health care system.” The latter is perhaps the big picture component that can include many things, but not ones that are necessarily incentivised under current funding.
http://healthit.hhs.gov/portal/server.pt?open=512&mode=2&objID=3541
Today, March 22, 2011 the ASQ’s Healthcare Update e-mail focused on Meaningful Use. The content is currently available at http://links.mkt3019.com/servlet/MailView?ms=OTcyNjg4S0&r=ODc0MzI5Mjc1S0&j=MjU4MzkzMDYS1&mt=1&rt=0
For a different take on Meaningful Use you might enjoy the humorous rap at the American College of Medical Informatimusicology web site. While perhaps not to everyone’s taste, it is at least tasteful.
http://informatimusicology.blogspot.com/2011/03/meaningful-yoose-rap-music-video-world.html
Will vendors have to receive new EHR Meaningful Use certification for stage 2 or will their previous certification still be valid?
A new proposed rule for Meaningful Use Stage 2 was released on February 23rd, 2012. Running a mere 455 pages, the proposed rule covers new and/or revised criteria for EMR incentive payments, and sets a new timetable for various milestones.
http://www.ofr.gov/OFRUpload/OFRData/2012-04443_PI.pdf
The final rules for Stage 2 EHR meaningful use were released on August 23, 2012. There are two parts. One is the CMS requirements for Meaningful Use. The other is the ONC requirements for EHR certification.
CMS - http://www.ofr.gov/OFRUpload/OFRData/2012-21050_PI.pdf
ONC - http://www.ofr.gov/OFRUpload/OFRData/2012-20982_PI.pdf
So meaningful use has a different meaning within the context of who is assessing it? There is no standard definition? How would medical device companies israel or from overseas handle this?